
FoxP1 (SP133)
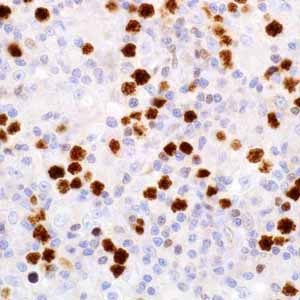
Diffuse large B-cell lymphoma (DLBCL), although considered a single category in the World Health Organization classification, most likely represents different clinicopathologic entities, which is difficult to separate using standard technique.1,2 From the clinical standpoint, the introduction of immunochemotherapy in the treatment of DLBCL has dramatically improved the outcome of these patients compared with chemotherapy alone.3,4 However, almost one-third of these patients become refractory or eventually relapse.5 Therefore, it is very important to identify and stratify biologic and/or clinical factors for patients who are at a higher risk for relapse. Gene expression profiling (GEP) studies have shown that diffuse large B-cell lymphoma (DLBCL) can be reproducibly divided into the prognostically important subtypes of germinal center B-cell-like (GCB), activated B-cell–like (ABC), and unclassified DLBCL.2,6,7 When treated with a regimen containing cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or other CHOP-like regimens (CHOP-treated), patients with GCB-DLBCL have a better survival independent of the International Prognostic Index.3-5,8 The prognostic value of GEP classification remains significant for DLBCL patients treated with rituximab plus CHOP or CHOP-like therapy (R-CHOP-treated).8 The GCB and ABC subtypes have different pathogenetic mechanisms that will impact the development of targeted therapies.6 Other GEP studies have also characterized primary mediastinal large B-cell lymphoma (PMBL) as distinct from the other subtypes of DLBCL and with a good prognosis similar to GCB-DLBCL.9 Despite the robustness of GEP in subclassifying DLBCL, GEP techniques are not applicable to the routine clinical practice due to the substantial time, technological expertise, and scarce resources required. Therefore, it is beneficial for the translational application of the GEP classification into protein expression by tumor cells to be developed through immunohistochemical (IHC) staining of formalin-fixed, paraffin-embedded tissues. Recently, different approaches using immunophenotypic algorithms with small panels of antibody biomarkers have been developed to translate the robust information from molecular studies into a routine clinical platform.10-14 A panel of antibodies: CD10, BCL6, MUM1/IRF4, GCET1, FoxP1, LMO2, and BCL2 has been used to determine the origin of GCB or non-GCB and each algorithm has different percentage thresholds for positive staining.10-14 In the Colomo’s algorithm10, the non-GCB phenotype was established if MUM1/IRF4 was positive (≥ 25% of tumor cells). The cases that were negative for MUM1/IRF4 and positive (≥ 25% of tumor cells) for CD10 were considered to be the GCB phenotype. Cases negative for MUM1/ IRF4 and CD10 and positive for BCL6 (≥ 25% of tumor cells) were also assigned to the GCB group. Finally, cases negative for the 3 markers were considered as not classified.10 In the Hans’ algorithm11, the tumors were assigned to the GCB phenotype if both CD10 and BCL6 were negative, the case was considered to be of non-GCB origin. If both BCL6 was positive and MUM1/IRF4 (≥ 30% of tumor cells) was positive, the case was assigned to non-GCB origin whereas if MUM1/IRF4 was negative (< 30% of tumor cells), then the case was assigned the GBC phenotype.11 The Hans algorithm had a high concordance with the GEP results (86%).11 According to the Muris’ algorithm12, cases positive (≥ 30% of tumor cells) for CD10 were assigned to the GCB phenotype. Cases negative for CD10 were differentiated according to MUM1/IRF4 (≥ 30% of tumor cells) expression into the ABC or the GCB phenotype. Thereafter, BCL2 immunostaining was used to separate 2 different prognostic groups (1 and 2).12 The 2 steps of the Muris’ algorithm were used to assess GCB versus ABC status and the prognostic impact of the algorithms was applied.12 Although the Muris’ algorithm had a relatively high concordance with the GEP results, it suffered low sensitivity and specificity. The Choi’s algorithm13 demonstrated that the cases positive for GCET1 (≥ 80% of tumor cells) and MUM1/IRF4 (≥ 80% of tumor cells) and/or FoxP1 (≥ 80% of tumor cells) or negative for CD10 and BCL6 (≤ 30% of tumor cells) were assigned to the non-GCB group. The cases positive for CD10 (≥ 30% of tumor cells), GCET1 (≥ 80% of tumor cells) without MUM1 expression, or positive for BCL6 without FoxP1 expression were classified as GCB.13 This study indicated the importance of FoxP1 in the subclassification of DLBCL. Choi et al then modified their approach to DLBCL subclassification by focusing on FoxP1. The tumors that are positive for FoxP1 and GCET1 are assigned to GCB subgroup, but, if FoxP1 positive and GCET1 are negative, the tumors belong to the ABC phenotype. If a case is FoxP1 negative but MUM-1/IRF4 positive, it still belongs to the ABC phenotype as long as CD10 is not expressed. This modified method emphasized the role of FoxP1, MUM1/IRF4, and GCET1 in the subclassification of DLBCL.15 The Choi’s algorithm had a very high concordance with the GEP results (87%).13, 15 In Nyman’s modified activated B-cell-like classification14, the cases expressing MUM1/IRF4 or FoxP1 were considered to belong to ABC subgroup, and the rest of the cases were assigned as GCB subtype. In the Tally algorithm described recently15, the method included an equal number of GCB markers (GCET1 and CD10) and non-GCB markers (FoxP1 and MUM1/IRF4). This algorithm was constructed from the immunophenotype pair with more positive antigens. Because two antibodies are used for each type, the LMO2 antigen determines the phenotype (GCB or non-GCB) when the score is equal in the two categories.15 Of these published algorithms, the Choi algorithm is the most predictive of GEP results and survival but is the least user-friendly. It requires the use of five antibodies, two of which are not commonly performed by most immunohistochemistry laboratories (GCET1 and FoxP1). Immunostains for BLC6 are technically difficult to perform and to interpret.11 Besides these problems, the Choi algorithm uses various cutoffs for determining antibody positivity and requires sequential interpretation of the results. An attempt to address some of these issues led to the examination of two additional algorithms. Because of the problems with BCL6, it was removed from the Hans algorithm, leading to a new algorithm (Hans*). The overall ability of the Hans* algorithm to predict the cell of origin and survival was similar to the original Hans algorithm. This minor difference in prognostic ability is offset by the ease of use of the modified Hans algorithm. Removal of BCL6 from the Choi algorithm, rearrangement of the order of antibody examination, and standardization of positivity (30% of the tumor cells) led to a new algorithm (Choi*) that was easier to use than the original and had a similar ability to predict the cell of origin and EFS. Prediction of OS, although statistically significant, was slightly decreased compared with the original algorithm; however, this decrease was offset by the ease of use. All of the algorithms have a similar feature: certain antibodies have precedence over others because of the order of examination. By removing the order of examination and scoring the results of four selected antibodies, a Tally algorithm was created. This Tally algorithm includes the GCB-specific antigens CD10 and GCET1 and the ABC-specific antigens MUM1 and FoxP1. The GCB-specific antigen LMO2 is only used as a tie-breaker to classify the tumor. The Tally algorithm shows a better ability to predict the cell of origin than any algorithm examined in this study. The Tally algorithm also divides DLBCL patients into two groups with significantly different OS and EFS. Although the Tally algorithm is the best for predicting the cell of origin, it too has drawbacks. First, it uses three antibodies that are commercially available but not commonly performed by many immunohistochemistry laboratories: GCET1, FoxP1, and LMO2. Second, the interpretation of GCET1, FoxP1, and LMO2 can be problematic, as some tumors show high background or nonspecific staining. Therefore, FoxP1 is useful in subclassification of DLBCL and a high cutoff (≥80%) for FoxP1 is needed to achieve high specificity for the ABC subtype.
